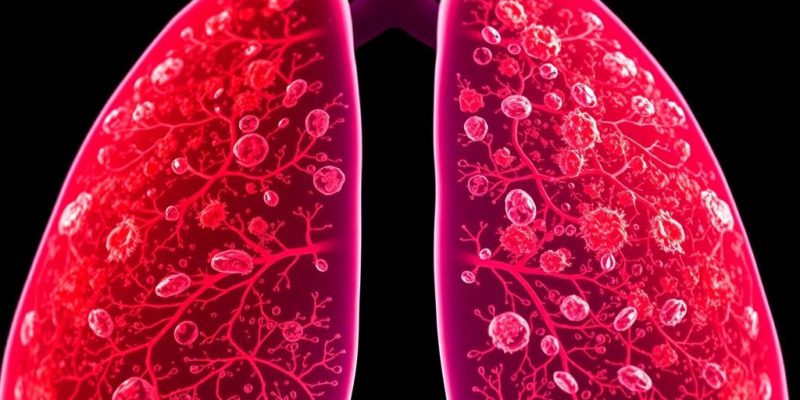
Cigarette Smoking
Cigarette smoking is, without a doubt, the leading cause of lung cancer. It’s pretty straightforward: the more you smoke, the higher your risk. The chemicals in cigarettes damage lung cells, making them more likely to turn cancerous. It’s not just about how many cigarettes you smoke a day, but also how long you’ve been smoking. Even light smokers are at risk, though the risk is lower than for heavy smokers. Quitting smoking, no matter how long you’ve smoked, can significantly reduce your risk of developing lung cancer. It’s never too late to quit, and there are tons of resources available to help people kick the habit. The decline in smoking prevalence has had a huge impact on lung cancer rates.
Cigar and Pipe Smoking
Okay, so maybe you don’t smoke cigarettes, but what about cigars or pipes? Well, they’re not exactly harmless either. While the risk might be slightly lower than with cigarettes, it’s still significantly higher than for non-smokers. Cigar and pipe smokers often inhale less smoke than cigarette smokers, but they’re still exposed to harmful chemicals. Plus, cigars tend to be larger and contain more tobacco than cigarettes, leading to greater exposure to carcinogens. It’s a common misconception that these are safer alternatives, but the truth is, they still pose a serious risk to your lung health. The risk of lung metastasis is still present with these forms of tobacco use.
Secondhand Smoke Exposure
Secondhand smoke is a real problem, even if you don’t smoke yourself. Breathing in someone else’s smoke can increase your risk of lung cancer. It’s especially dangerous for children, who are more vulnerable to the effects of secondhand smoke. Secondhand smoke contains the same harmful chemicals as the smoke inhaled by smokers. It’s a mix of smoke from the burning end of a cigarette, cigar, or pipe, and the smoke exhaled by the smoker. Avoiding exposure to secondhand smoke is important for protecting your lung health. Here are some ways to reduce exposure:
- Avoid smoky environments.
- Ask smokers to smoke outside.
- Support smoke-free policies in public places.
Environmental Factors Contributing To Lung Cancer
It’s not just smoking that causes lung cancer; the environment plays a big role too. Things we breathe in or are exposed to daily can really increase the risk. It’s kind of scary when you think about it – stuff you can’t even see could be harming you. Let’s break down some of the main environmental culprits.
Air Pollution
Air pollution is a major concern, especially in cities. The tiny particles and gases in polluted air can damage your lungs over time. Think about it: every breath you take in a polluted area is potentially harmful. It’s not just car exhaust either; industrial emissions and even dust can contribute. It’s a complex mix, and long-term exposure is what really increases the risk. You can learn more about air pollution’s impact on lung health.
Radon Gas Exposure
Radon is a naturally occurring gas that you can’t see or smell, and it comes from the ground. It can seep into homes and buildings, and prolonged exposure is linked to lung cancer. It’s actually the second leading cause of lung cancer in the US, after smoking. Testing your home for radon is super important, especially if you live in an area known for high radon levels. Mitigation systems can help reduce radon levels if they’re too high. Radon is especially dangerous for non-smokers.
Asbestos and Other Carcinogens
Asbestos is a mineral that was once widely used in construction. When asbestos fibers are inhaled, they can cause serious lung problems, including lung cancer and mesothelioma. Other carcinogens, like arsenic, chromium, and nickel, can also increase the risk of lung cancer, especially in occupational settings. It’s important to be aware of these risks and take precautions to minimize exposure. Here are some key points:
- Asbestos exposure is particularly dangerous.
- Occupational exposure to carcinogens requires strict safety measures.
- Regulations aim to limit exposure to these harmful substances.
Genetic Predisposition To Lung Cancer
It’s easy to think that lung cancer is all about smoking, but genetics play a bigger role than many realize. Some people are just born with a higher risk, thanks to the genes they inherit. It’s not a guarantee they’ll get the disease, but it definitely tips the scales.
Family History of Lung Cancer
If lung cancer runs in your family, it’s worth paying attention. Having a close relative with the disease can increase your own risk. It doesn’t mean you’re destined to get it, but it does mean you should be extra careful about other risk factors, like smoking or exposure to radon. I remember reading about a family where several members developed lung cancer, even though some of them never smoked. It really highlights how family history can be a significant factor. It’s not just about direct inheritance; shared environments and lifestyle choices within families can also contribute.
Inherited Genetic Mutations
Certain genetic mutations can significantly increase the risk of lung cancer. These mutations, like BRCA1/2 mutations, affect how cells repair damage and can make them more susceptible to becoming cancerous. It’s like having a built-in weakness. These mutations aren’t super common, but they can have a big impact on those who have them. Genetic testing can identify these mutations, but it’s not something everyone needs to do. It’s usually recommended for people with a strong family history of cancer. I’ve heard stories about people who discovered they had these mutations and then took proactive steps to manage their risk, like getting regular screenings or making lifestyle changes.
Ethnic and Racial Disparities
Lung cancer doesn’t affect everyone equally. There are noticeable differences in incidence and outcomes across different ethnic and racial groups. For example, some studies have shown that certain populations may have a higher prevalence of specific genetic variations that increase their susceptibility to lung cancer. Socioeconomic factors and access to healthcare also play a role, but genetics can’t be ignored. It’s a complex issue with many layers. Understanding these disparities is crucial for developing targeted prevention and treatment strategies. I think it’s important to acknowledge these differences and work towards more equitable healthcare for everyone. Research like this study is helping us understand the genetic factors at play.
Here are some factors that contribute to ethnic and racial disparities:
- Genetic predispositions
- Environmental exposures
- Access to healthcare
Occupational Hazards Linked To Lung Cancer
It’s easy to forget that your job can seriously mess with your health, especially when it comes to lung cancer. Some professions come with a higher risk because of the stuff people are exposed to every day. It’s not just smoking that’s the problem; what you breathe in at work can be just as bad, or even worse. Certain jobs dramatically increase the risk of developing lung cancer due to exposure to harmful substances.
Exposure to Carcinogenic Substances
Think about it: miners breathing in all sorts of dust, construction workers dealing with asbestos, or factory employees handling chemicals. These aren’t just minor irritants; they’re carcinogens that can seriously damage your lungs over time. It’s kind of scary when you realize that something meant to provide a living could also be slowly killing you. Occupational exposure to secondhand smoke in environments like bars, casinos, and restaurants significantly raises the risk of lung cancer for workers.
Workplace Safety Regulations
You’d hope there are rules in place to protect workers, right? Well, there are, but they’re not always followed or enforced as well as they should be. Companies are supposed to provide protective gear, monitor air quality, and train employees on how to handle dangerous materials safely. But sometimes, corners get cut, and workers end up paying the price with their health. It’s a constant battle to make sure these regulations are actually doing their job. Cigarette smoking is the leading risk factor for lung cancer, responsible for approximately 80% to 90% of lung cancer deaths in the United States.
High-Risk Occupations
So, which jobs are the worst offenders? Here are a few:
- Miners: Constant exposure to radon and silica dust.
- Construction Workers: Asbestos and other building materials.
- Factory Workers: Various chemicals and industrial byproducts.
- Welders: Metal fumes.
- Firefighters: Smoke and toxic fumes from burning materials.
It’s a pretty grim list, and it highlights how important it is to be aware of the risks and push for better safety measures in these industries.
Lifestyle Choices Beyond Tobacco
It’s easy to think smoking is the only lifestyle factor that matters for lung cancer, but that’s not true. Other choices can play a role, too. Let’s take a look at some of them.
Diet and Nutrition
What you eat matters. A lot. There’s no magic food that prevents lung cancer, but a balanced diet can help. Eating plenty of fruits and vegetables is generally a good idea. Some studies suggest that diets high in processed meats might increase cancer risk, so maybe cut back on those?
- Focus on whole foods.
- Limit processed foods.
- Stay hydrated.
Physical Activity Levels
Getting enough exercise is important for overall health, and it might also help lower your risk of lung cancer. It’s not just about preventing cancer, though. Regular physical activity can improve your heart health, boost your mood, and help you maintain a healthy weight. Healthy weight is important for many reasons, including cancer prevention.
- Aim for at least 150 minutes of moderate-intensity exercise per week.
- Find activities you enjoy to make it easier to stick with it.
- Even small amounts of physical activity can make a difference.
Alcohol Consumption
Drinking too much alcohol isn’t good for you, and it might increase your risk of certain cancers, including lung cancer. It’s all about moderation. If you do drink, do so responsibly. Avoiding harmful substances is always a good idea.
- Limit alcohol intake to one drink per day for women and two drinks per day for men.
- Consider cutting back or quitting altogether.
- Be aware of the potential risks associated with alcohol consumption. Moderation is key.
Chronic Lung Diseases And Their Role
It’s pretty obvious that smoking is bad for your lungs, but what about other lung problems? Turns out, having certain chronic lung diseases can also increase your risk of getting lung cancer. It’s not a direct cause, but more like these conditions create an environment where cancer is more likely to develop.
Chronic Obstructive Pulmonary Disease (COPD)
COPD, which includes conditions like emphysema and chronic bronchitis, is a big one. People with COPD often have damaged lungs, making them more vulnerable. The constant inflammation and tissue damage can lead to abnormal cell growth, which, over time, can turn into cancer. It’s like the lungs are already struggling, and then cancer decides to join the party. It’s important to understand the lung adenocarcinoma risks associated with pre-existing conditions.
Pulmonary Fibrosis
Pulmonary fibrosis is another condition where the lung tissue becomes scarred and thickened. This scarring makes it harder to breathe and can also increase the risk of lung cancer. The exact reasons aren’t fully understood, but it’s thought that the scarring process itself can trigger changes in the cells that lead to cancer. It’s like the lungs are trying to repair themselves, but the repair process goes wrong. Here are some things to keep in mind:
- The scarring can distort the lung structure.
- It can create an environment where cancer cells thrive.
- It can make it harder to detect cancer early.
Tuberculosis and Lung Health
Tuberculosis (TB) is an infectious disease that usually attacks the lungs. While TB itself isn’t directly linked to lung cancer, the damage it causes to the lungs can increase the risk. TB can leave scars and inflammation, similar to pulmonary fibrosis, which can then lead to cancer. It’s like TB weakens the lungs, making them more susceptible to other problems, including cancer. It’s important to consider risk factors when assessing lung health.
So, if you have any of these chronic lung diseases, it’s super important to get regular check-ups and screenings. Catching lung cancer early can make a huge difference in treatment outcomes. It’s all about staying proactive and taking care of your lungs!
Age And Its Influence On Lung Cancer Risk
It’s no secret that getting older changes a lot about your body, and unfortunately, that includes your risk for diseases like lung cancer. Age plays a pretty big role, and it’s something worth understanding.
Age-Related Cellular Changes
As we age, our cells go through changes. Think of it like this: a brand new car runs smoother than one that’s been on the road for decades. The same goes for our cells. Over time, they can accumulate damage, making them more prone to becoming cancerous. This cellular wear and tear is a key factor in why older folks are more susceptible to lung cancer. It’s not just one thing, but a combination of factors that build up over the years. For example:
- DNA repair mechanisms become less efficient.
- The immune system weakens, making it harder to fight off abnormal cells.
- Cells are exposed to more carcinogens over a longer period.
Incidence Rates by Age Group
If you look at the numbers, it’s pretty clear: lung cancer is more common in older adults. The median age at diagnosis is around 70, which tells you something. It doesn’t mean younger people can’t get it, but the risk definitely increases as you get older. Adenocarcinoma prevalence is a key factor in lung cancer demographics. Here’s a quick breakdown:
- The risk starts to climb significantly after age 50.
- The highest rates are typically seen in people over 65.
- Younger people can get lung cancer, but it’s less common.
Screening Recommendations for Older Adults
Because age is such a big risk factor, screening is often recommended for older adults, especially those with a history of smoking. The idea is to catch the cancer early, when it’s easier to treat. It’s not a perfect system, but it can make a big difference. The median diagnosis ages for various cancers highlight the importance of age-related screening. Some things to keep in mind:
- Screening usually involves a low-dose CT scan.
- It’s generally recommended for people aged 50-80 who have a significant smoking history.
- Talk to your doctor to see if screening is right for you. Early detection can save lives.




Comments